INDICATION
TRUVADA FOR PrEP® (pre-exposure prophylaxis) is indicated to reduce the risk of sexually acquired HIV-1 in adults and adolescents (≥35 kg) who are at risk for HIV. HIV-1–negative status must be confirmed immediately prior to initiation
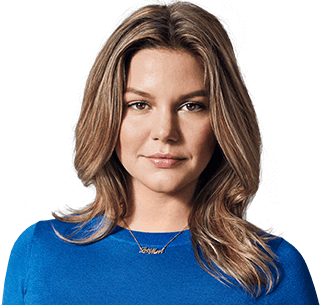
Empower women to help protect themselves from HIV
Inform them of all their options, including TRUVADA for pre-exposure prophylaxis (PrEP), available in the US since 20121
- TRUVADA FOR PrEP is a single tablet, taken once daily, that contains two active ingredients—tenofovir disoproxil fumarate (TDF) and emtricitabine (FTC)2
- It is approved to significantly reduce the risk of sexually acquired HIV-1 in individuals at risk2,3
- It is an HIV prevention option that does not depend on a male partner's cooperation4
- HIV-1–negative status must be confirmed immediately prior to initiating TRUVADA FOR PrEP and at least every 3 months thereafter2
US and global health guidelines recommend TRUVADA FOR PrEP5-9
in combination with safer sex practices to help reduce the risk of sexually acquired HIV-1 in individuals at risk
Health guidelines recommend TRUVADA FOR PrEP and emphasize the importance of counseling on adherence and HIV-1 risk reduction strategies5-9
Learn about identifying women at risk for HIVINDICATION
TRUVADA FOR PrEP (pre-exposure prophylaxis) is indicated to reduce the risk of sexually acquired HIV-1 in adults and adolescents (≥35 kg) who are at risk for HIV. HIV-1–negative status must be confirmed immediately prior to initiation
IMPORTANT SAFETY INFORMATION
BOXED WARNING: RISK OF DRUG RESISTANCE WITH USE OF TRUVADA FOR PrEP IN UNDIAGNOSED EARLY HIV-1 INFECTION and POST TREATMENT ACUTE EXACERBATION OF HEPATITIS B
- TRUVADA FOR PrEP must be prescribed only to patients confirmed to be HIV negative immediately prior to initiation and at least every 3 months during use. Drug-resistant HIV-1 variants have been identified with use of TRUVADA FOR PrEP following undetected acute HIV-1 infection. Do not initiate if signs or symptoms of acute HIV-1 infection are present unless HIV-negative status is confirmed
- Severe acute exacerbations of hepatitis B virus (HBV) have been reported in patients who have HBV infection and discontinued TRUVADA. Hepatic function should be monitored closely with both clinical and laboratory follow-up for at least several months in patients with HBV after discontinuing TRUVADA. If appropriate, initiation of anti-hepatitis B therapy may be warranted
Contraindication
- TRUVADA FOR PrEP is contraindicated in patients with unknown or positive HIV status
Warnings and precautions
- Comprehensive management to reduce risks:
- Use TRUVADA FOR PrEP to reduce the risk of HIV-1 infection as part of a comprehensive strategy that includes adherence to daily dosing and safer sex practices, including condoms, to reduce the risk of sexually transmitted infections (STIs)
- HIV-1 risk factors: Behavioral, biological, or epidemiologic HIV-1 risk factors may include, but are not limited to condomless sex, past or current STIs, self-identified HIV risk, having sexual partners of unknown HIV-1 viremic status, or sexual activity in a high-prevalence area or network
- Reduce STI risk: Counsel on the use of STI prevention measures (e.g., consistent and correct condom use, knowledge of partner’s HIV-1 status, including viremic status, regular testing for STIs)
- Reduce potential for drug resistance: Only prescribe TRUVADA FOR PrEP to patients confirmed to be HIV negative immediately prior to initiation, at least every 3 months while taking TRUVADA, and upon an STI diagnosis. HIV-1 resistance substitutions may emerge in patients with undetected HIV-1 infection who are taking only TRUVADA because TRUVADA alone is not a complete regimen for treating HIV-1
- Some HIV tests may not detect acute HIV infection. Prior to initiating TRUVADA FOR PrEP, ask patients about potential recent exposure events. If recent (<1 month) exposures are reported or suspected, or symptoms of acute HIV infection (e.g., fever, fatigue, myalgia, skin rash) are present, confirm HIV-negative status with a test approved by the FDA for use in the diagnosis of acute HIV infection
- If HIV-1 infection is suspected or if symptoms of acute infection are present while taking TRUVADA FOR PrEP, convert the TRUVADA FOR PrEP regimen to a complete HIV treatment regimen until HIV-negative status is confirmed by a test approved by the FDA for use in the diagnosis of acute HIV infection
- Counsel on adherence: Counsel patients to strictly adhere to daily dosing, as efficacy is strongly correlated with adherence. Some patients, such as adolescents, may benefit from more frequent visits and counseling
Warnings and precautions
- New onset or worsening renal impairment: Cases of acute renal impairment and Fanconi syndrome have been reported with the use of TDF. TRUVADA is not recommended in patients with estimated creatinine clearance (CrCl) <60 mL/min. Avoid concurrent or recent use with a nephrotoxic agent. Acute renal failure has been reported after initiation of high-dose or multiple NSAIDs in patients at risk for renal dysfunction; consider alternatives to NSAIDs in these patients. Monitor renal function in all patients (see Dosage and Administration section)
- Bone effects: Decreases in bone mineral density (BMD) and mineralization defects, including osteomalacia associated with proximal renal tubulopathy, have been reported with the use of TDF. Consider monitoring BMD in patients with a history of pathologic fracture or risk factors for bone loss
- Lactic acidosis and severe hepatomegaly with steatosis: Fatal cases have been reported with the use of nucleoside analogs, including TRUVADA. Discontinue use if clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity develop, including hepatomegaly and steatosis in the absence of marked transaminase elevations
- Drug interactions: See Drug Interactions section. Consider the potential for drug interactions prior to and during use of TRUVADA, and monitor for adverse reactions
Adverse reactions
- Common adverse reactions (>2% and more frequently than placebo) of TRUVADA FOR PrEP in clinical trials were headache, abdominal pain, and weight loss
Drug interactions
- Prescribing information: Consult the full Prescribing Information for TRUVADA for more information, warnings, and potentially significant drug interactions, including clinical comments
- Hepatitis C antivirals: Coadministration with ledipasvir/sofosbuvir, sofosbuvir/velpatasvir, or sofosbuvir/velpatasvir/voxilaprevir increases TDF exposure; monitor for adverse reactions
- Drugs affecting renal function: Coadministration of TRUVADA with drugs that reduce renal function or compete for active tubular secretion may increase concentrations of emtricitabine and/or tenofovir
Pregnancy and lactation
- Pregnancy: An Antiretroviral Pregnancy Registry (APR) has been established. Available data from observational studies and the APR show no significant difference in the rate of major birth defects for TRUVADA compared with a US reference population. Consider HIV prevention methods, including TRUVADA FOR PrEP in women due to the potential increased risk of HIV-1 infection during pregnancy and mother-to-child transmission during acute HIV-1 infection
- Lactation: Emtricitabine and tenofovir have been detected in human milk. Evaluate the benefits and risks of TRUVADA FOR PrEP in breastfeeding women, including the risk of HIV-1 acquisition due to nonadherence, and subsequent mother to child transmission. Health benefits of breastfeeding should be considered along with potential adverse effects of TRUVADA on the child, which are unknown
Dosage and administration
- Dosage: One tablet, once daily, with or without food
- HIV screening: Test for HIV-1 infection prior to initiating and at least every 3 months during treatment
- HBV screening: Test for HBV infection prior to or when initiating treatment
- Renal impairment and monitoring: Not recommended in patients with CrCl <60 mL/min. Prior to or when initiating TRUVADA, and during use on a clinically appropriate schedule, assess serum creatinine, CrCl, urine glucose, and urine protein in all patients. In patients with chronic kidney disease, assess serum phosphorus
Please see full Prescribing Information for TRUVADA FOR PrEP, including BOXED WARNING.
References: 1. US Food and Drug Administration. Truvada for PrEP fact sheet: ensuring safe and proper use. Created July 2012. Accessed July 23, 2020. https://www.fda.gov/downloads/drugs/drugsafety/postmarketdrugsafetyinformationforpatientsandproviders/ucm312290.pdf 2. Truvada. Package insert. Gilead Sciences, Inc.; 2020. 3. Baeten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399-410. 4. Bradley ELP, Hoover KW; Centers for Disease Control and Prevention Women and PrEP Discussion Series Team. Improving HIV preexposure prophylaxis implementation for women: summary of key findings from a discussion series with women's HIV prevention experts. Womens Health Issues. 2019;29(1):3-7. 5. The American College of Obstetricians and Gynecologists Committee on Gynecologic Practice. Committee Opinion No 595: Preexposure prophylaxis for the prevention of human immunodeficiency virus. Obstet Gynecol. 2014;123(5):1133-1136. 6. World Health Organization. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV, September 2015. Published June 2016. Accessed July 23, 2020. https://apps.who.int/iris/bitstream/handle/10665/186275/9789241509565_eng.pdf?sequence=1 7. Centers for Disease Control and Prevention. Preexposure prophylaxis for the prevention of HIV infection in the United States–2017 update: a clinical practice guideline. Published March 2018. Accessed July 23, 2020. http://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf 8. Saag MS, Benson CA, Gandhi RT, et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults: 2018 recommendations of the International Antiviral Society-USA Panel. JAMA. 2018;320(4):379-396. 9. American College Health Association. ACHA Guidelines: HIV Pre–exposure Prophylaxis. Published January 2019. Accessed July 23, 2020. https://www.acha.org/documents/resources/guidelines/ACHA_HIV_PrEP_Guidelines_Jan2019.pdf